II. Clinic Information
Malpractice Insurance
Malpractice Insurance is provided by the program and is only for patient care provided in the school.
Communication Policy
- Residents are required to provide a contact number (cell phone number is preferred). There is no overhead pager system.
- Residents should respond to pages promptly (ideally within 5 minutes, more than 15 minutes is considered not answered).
- Residents will be provided with a University of Maryland e-mail address which will become the official e-mail address for Program communication.
- Residents should review their University of Maryland e-mail account at least once a day and Friday afternoon before leaving work. E-mail will be the primary source of non-urgent communication.
After Hours Emergencies - Responsibilities
- All residents must be accessible (24 hours/7days a week) in order to manage treatment of your emergency patients during non-clinic hours (cell phone number is preferred).
- Handle all “emergency” telephone inquiries from your assigned patients (provide a referral if necessary or a prescription).
- Contact either Dr. Barnes (443.271.2194) or Ms. Chenowith (443.504.8292) for assistance as required.
- The next work day, after the emergency care, the AEGD Office Manager will pull the chart to ensure that the resident makes an entry and have it co-signed by a faculty member.
Operating Hours for AEGD Clinic
- Patient appointments are 8 am to 4 pm,. Residents are required to arrive by 7:30 am and not to depart until 4:30 pm.
- CLINIC Schedule
First Patient – 8 am to 9:30 am
Second Patient – 9:30 am to 11 am
Third Patient – 11 am to 12 noon
LUNCH – 12 pm to 1 pm
Fourth Patient – 1 pm to 2:30 pm
Fifth Patient – 2:30 pm to 4 pm
Scheduling of Emergency Patients
- If emergency patient is assigned to a resident, anyone in the TEAM will see the patient if there is an opening.
- Emergency patients will be given any empty slot in the appointment schedule with any available resident.
- If there is no empty slot, the TEAM captain will decide who will see the patient.
Treatment Plans
- All treatment plans must be reviewed by an attending and signed by the patient, resident and attending before any restorative treatment can begin.
- In treatment planning cases, especially if they are complex, residents must first collect all necessary data, including mounted diagnostic casts. Sometimes, diagnostic wax-ups may be required and patient can be charged for it. There is no charge to the patient if the wax-up is done for the resident’s benefit, unless wax-up is done by outside laboratory (only if approved by the faculty).
- Format for treatment planning is discussed in Introduction to Treatment Planning Technical Criteria.
- Residents are expected to have a treatment plan written out before approaching an attending for evaluation. By presenting the case in such a manner, a more meaningful discussion will emerge. Always bring mounted casts, x-rays and the chart for treatment planning.
- A sequenced treatment plan should be written after final attending approval and discussion.
- All treatment plans must be entered into Axium and swiped by attending faculty.
- When a comprehensive treatment is completed and prior to entering the patient into the stem, a chart audit (record review) and case complete audit must be performed (see Case Complete Form Instructions).
Medical Consults
For medically compromised patients where dental treatment plans will need to be altered due to patient condition, a medical consult form must be filled out. Residents will send the information request via the patient to the medical doctor. The patient will then return the form to the resident and it will be added to the patient’s dental chart. See example of a medical consult form. Any ASA III and IV patient requires a medical consult and medical clearance prior to dental treatment.
When residents are phoning medical doctors for patient consults, it is advised that the resident prepare in advance what to say. In general, the resident should include the following:
- Identify yourself (DDS, Dental Resident at UMAB) and your patient.
- State the known health condition of the patient.
- Describe the dental procedures planned. Medical doctors tend not to have a detailed understanding of these procedures; thus, account the details of the surgery, the extent of bleeding predicted, the intended local anesthetic or medication to be used, and/or the possible effects of the dental treatment on the patient.
- Specifically ask the information required from the medical doctor. Examples: “Should antibiotic prophylaxis be administered prior to dental therapy?” “Is the use of epinephrine in the local anesthetic contraindicated?” Avoid asking too general a question like, “Is there anything that should concern me about the patient?”
- Document discussion in the Progress Notes of the patient’s record and ask for written documentation from attending physician.
Medical Updates
Medical updates form should be completed for every patient who has not been in the AEGD Clinic in the last one year and shall be co-signed by a faculty member. It should be resident’s customary question to ask about any changes in patient’s medical condition at every visit.
Dental Hygiene
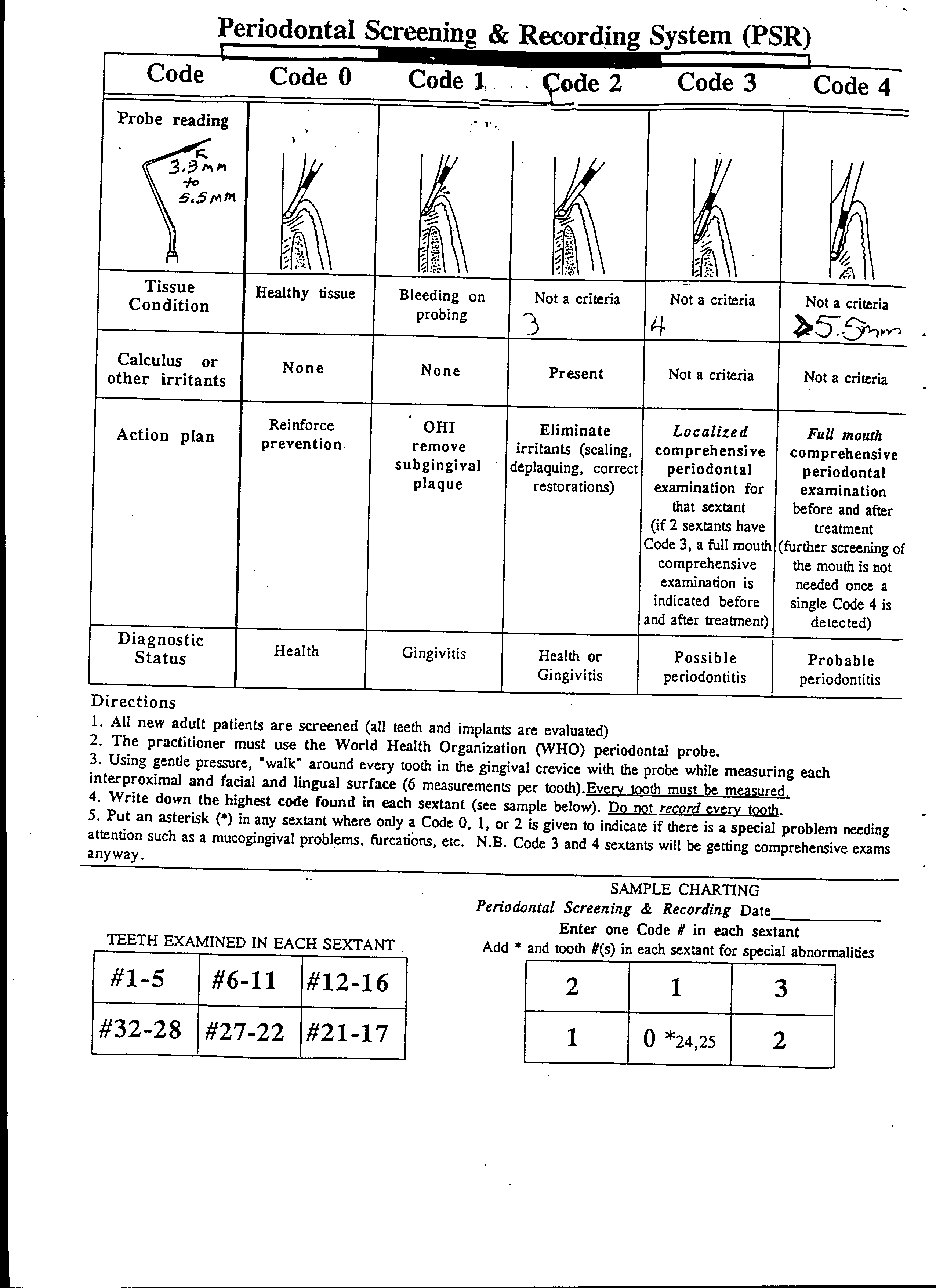
An integral part of the AGD family are the hygienists; they provide oral care instructions, prophylaxis treatment, debridements, and fluoride treatments and placement of Arestin. These services are available via (1) completed prescribed treatment plans and/or (2) appointed recall visits with the hygienist. Treatment plans are to be comprised of full mouth probings and chartings and radiographs annually. During the recall, the hygienists uses the PSR system for record bleeding points (see Periodontal Screening & Recording System (PSR)).
Hygiene visits can commence prior to or in conjunction with restorative appointments. At completion of the hygiene visit a recall card is completed to be mailed at the appropriate interval as a reminder for the patient. There are also hygiene products available for application or by prescription or for purchase via the clinic.
AEGD Dental Assistants
We, the assistants welcome you to AEGD. We are looking forward to working with you during this next year. Listed below are items that you can expect from us as a group each and every day:
| I. |
Chair Setup – You will be completely setup for your patient (cassette, medicaments, disposable handles, etc.). This can only be accomplished with schedules posted and procedures noted. During the course of the day, residents could be expected to cleanup and setup their own chairs. |
| II. |
Chairside Assisting – There is not an assistant for each resident. Assistants will be able to help residents during the critical part of the procedure. (Mixing and placing of amalgams, mixing impression materials, placing of composites, etc.). Surgeries always have first priority. |
| III. |
Screening – If a resident is doing screening on any day, the assistant in that zone will help with the charting. The resident will be expected to take the necessary radiographs. |
| IV. |
Radiographs – Assistants will take PA’s and BW if available. Residents will take FMS. |
| V. |
Rubber Dam – The assistants are asking the residents to use the rubber dam whenever they can. This will help the resident during the procedure, especially when they won’t have an assistant available. |
| VI. |
Become Familiar with Layout – We are asking residents to know what is in cluster cabinets in your zones and what is in the drawers at your chairs. |
Clinic Coordinator
The Clinic Coordinator provides patient support services that are both efficient and caring.
- Acts as a patient advocate, acquainting patients with policies and procedures relevant to their care and helping them navigate the system as necessary. Provides excellent customer service to internal and external calls regarding information, treatment and special needs. Responds to patient concerns and forwards concerns to the program director as necessary.
- Provides individualized coordination of care; when necessary, reviews chart to monitor patient clinical progress.
- Assesses outcomes of care; analyze complaints to determine trends. Surveys patient via questionnaires; resolve complaints.
- Assists students with patient management.
Communication and Teamwork
These are the items you can expect from the assistant on a day-to-day basis. The key to a great relationship between residents and assistants is communication. Talk to your assistant. Let them know if there is a change in your schedule. Communicate to them what time you will really need their assistance. The more we talk to one another, the easier the day will flow.
Production Report
This report is given monthly to the resident to monitor procedures completed by ADA codes. The resident is responsible for maintaining the record in their portfolio. (See Production Report.)
Exposure Reporting and Management Procedure, Baltimore Campus
If an exposure has or may have occurred:
- STOP and IMMEDIATELY remove item responsible for exposure to prevent a DOUBLE exposure
- Note if item is visibly bloody.
- Remove PPE and set aside gloves for checking later if a glove breach is not obvious (SOD nurse can help with this).
- Wash all wounds with soap and water, and flush exposed mucous membranes with cool water
- Do not force wounds to bleed
- DO NOT dismiss source patient/stop patient from leaving (if possible)
- Prepare to report the incident, make note of patient medical history/risk factors and have patient ID #
- Report incident to your attending faculty (student/resident), or department supervisor (staff)
- Report exposure to an SOD nurse; the most efficient way to do so is to use the emergency pager system
- To place an emergency page:
- Locate the button marked Emergency on a clinic wall phone and press (emergency pager number will be auto dialed) or dial 410-389-1324 (dial 9 first if using an SOD phone)
- After 3 beeping tones are heard, enter your room or quad number, followed by the # sign (lower level dial 777)
- Nurse(s) will respond to your area within a few minutes (page again, if no response in 3-5 minutes)*
* If unable to contact SOD nurse, phone the University of Maryland Immediate Care, Bloodborne Pathogen Exposure Hotline (BBPE Hotline) at 667-214-1886; if using an SOD phone, dial 9 first. DO NOT go to the ER without a referral from Dr. Baronas or a member of his staff.
- Complete the required forms (all incident details must be provided to an SOD nurse as soon as possible)
Required Injury Reporting Forms:
- Student/Resident, Staff, Employee and Volunteer forms will be provided by a SOD nurse, or can located in bins on SOD nurses’ office doors
| Students |
Employees* (Staff and Faculty) |
Volunteers |
1) U of MD Post Occupational Exposure Information Sheet
2) Adverse Incident Report (done by SOD nurse) |
1) First Report of Injury (needed for medical follow-up)
2) Accident Witness Statement (indicate if no witness)
3) Supervisor’s report of Injury *department must fax to corporate or state EHS within 3 days (copy to SOD nurse), unless done online
4) U of MD SOD Post Occupational Exposure Information Sheet
5) Adverse Incident Report (done by SOD nurse) |
1) U of MD SOD Post Occupational Exposure Information Sheet
2) JE Authorization Form (needed to receive treatment at U of MD Immediate Care
3) Adverse Incident Report (done by SOD Nurse) |
Adverse Incident Forms (old format) in bin on nurses’ doors and can be used to record the facts, or write the details on paper until a nurse can enter them online. Never refer to an incident report in the EPR; record incident facts only.
J. Naglik, RN 4/12/2016
Medical Emergency Response Protocol
For Immediate Life-threatening Emergencies or Behavioral Incidents:
- During Normal Business Hours (Mon-Fri 8:00AM – 5:00 PM; Tue, Wed and Thurs (C-3 Clinic) 5:00PM – 7:00 PM:
(1) Use a clinic phone to call Campus Police by dialing 711 (DO NOT dial 9 first). Campus Police will call for an ambulance if needed, and/or send officers to assist.
(2) Always follow a call to campus police with a page of the School of Dentistry Emergency response page (see Protocol for Dental School Emergency Response Team Paging /Response described below)
- When there is no nurse coverage in the evening or no nurse available during the daytime, attending faculty will manage the incident:
- Use clinic phones to call 711 (campus police will call for an ambulance or come to assist as needed).
- Report the incident to a Dental School nurse verbally or by email at the earliest opportunity.
Protocol for Dental School Emergency Response Team (ERT) Paging / Response:
- Press the button labeled “Emergency” on a clinic wall phone pre-programmed to page the ERT
- From a non-clinic phone within the building, page using the number 9-410-389-1324
- After triple beep tone, enter the nearest room/quad # where the emergency is occurring (ground or lower level, and large areas without a clear room number like reception rooms, follow pink emergency response signs near area phones).
- Emergency responders will report to the area received on the pager and provide treatment if available. If no response within 5 minutes page again to rule out pager malfunction, and always refer to attending faculty for guidance. It may be that all emergency responders are otherwise engaged.
Before Responders Arrive:
- If bodily fluids present and/or victim is coughing, don the appropriate PPE where available
- first responder will act as “captain” and direct interventions until a more qualified or experienced individual arrives to take over that role.
- Position victim so as to protect from further injury on the floor or in a dental chair.
- If campus police have been called to send an ambulance, designate a person to alert the guard in the atrium lobby, and to assist the EMTs to the location of the emergency.
- Bring, or have someone bring the Emergency Cart/Oxygen tank into the room/quad (located outside clinic prep area or in some side hallways off main corridors).
- Start oxygen with a nasal cannula for oxygen support at 2-4 L/min, or with a non-rebreather mask, or if the patient is distressed due to shortness of breath, at 10- 15L/min (make sure bag attached to the non-rebreather mask inflates).
- Provide treatment if trained; Do not wait for emergency responders, if basic life support is needed (See basic CPR instructions from the AHA in the front of white emergency binders on top of red Emergency Cart if necessary).
Using the Emergency Response Team for Non-Life-Threatening Emergencies:
- Page the Dental School Emergency Response Team only, not campus police
For A Glucometer Test or Blood Pressure Verification on an Asymptomatic Patient:
- Members of the Emergency response team can be paged individually at pager numbers listed below. Nurses are to be paged before the Doctor.
Members of the Emergency Response Team include, but are not limited to the following individuals who will be alerted when the emergency pager number 9-410-389-1324 is activated:
| |
Personal Pager # |
Phone # |
Room |
| 1. RN II (Oral Surgery Nurse) |
(9-410-389-1334) |
6-4026 |
1326 |
| 2. RN II (Infection Control Nurse) |
(9-410-389-1298) |
6-6344 |
4317 |
| 3. LPN (Dental School Nurse) |
(9-410-389-1331) |
6-7496 |
2318 |
| 4. Dr. Idzik-Starr |
(9-410-389-1332) |
6-4010 |
OMS |
| 5. Dr. Leventer |
(9-410-389-0729) |
6-2470 |
3217 |
Laboratories
Professional Labs
- Friendship, Empire and Americus dental labs handle the Dental School’s fixed and removable prosthodontic cases.
- Microdental Lab may be used for involved esthetic cases.
Lab Prescriptions
- Please make sure all necessary information is present in the prescription for the lab to complete the case. Residents sign the prescription and then it must be countersigned by the attending faculty.
- Laboratory prescriptions must also have the signature of the office manager in order to ensure that a minimum of 50% payment was made. The lab will not process the case without these signatures, nor will they do so without the patient name and chart number.
- Any laboratory prescription involving new technology products and an alternative laboratory should be approved by the Director.
The Dental School is moving towards an electronic lab tracking system which the AEGD program is testing. Access Axium Links for up-to-date information.
Dental Lab Cases
- All lab work for AEGD department is submitted to the Dental School in-house labs. This work will be routed to an outside lab. Any case that needs to be glazed and polished will be completed in the in-house lab.
- Lab pans are used to store active lab cases going to removable and fixed labs. When the case is delivered, please empty and return the lab pan. All old models, impressions, yellow and white prescription forms should be thrown away.
- The AEGD department uses the Dental School prescription form. All copies should be attached to the lab pan. All cases must be signed out before going to the dental labs (4:00 pm on prior day).
- All impression, wax and metal try-in’s must be disinfected before going to the labs and indicated on prescription form.
- Cases that are ready to be sent to the lab, should be placed in bags and left on the lab cart inside the clinic conference room #2312.
- All lab cases must be signed by a faculty member and the office manager, prior to being sent out to the lab.
- Fixed, Remo and Ortho lab cases are delivered and picked up once a day at approximately 9 a.m.
- Incoming lab cases are signed in; then placed on the lab cart inside the clinic conference room #2312.
- To expedite the process of having your case returned to you as quickly as possible, please be sure to include the date forward, the date of return, and the clinic’s letters (AEGD) on your prescription form. Also, start your day count for your case to be returned on the next working day. Don’t forget to exclude holidays and clinic closings.
- Mr. Rick Baier is the Dental School’s Prosthodontics Lab Supervisor.
- Name and date all study models.
- Check your lab shelf at least twice a day, every day for returned lab cases for dies that need to be trimmed, MD Bridge designs, RPD designs, etc.
- Prepare for patients who may need lab work at their next appointment by checking your patient schedule, and their charts at least 2 days prior to their next appointment.
Infection Control
- Note that impressions MUST be properly disinfected and bagged prior to delivery to the labs. The laboratory form must be labeled “disinfected”.
- Remove gloves and wash hands BEFORE entering the lab area.
Time Required
- Both fixed and removable cases require pre-set working days depending on the complexity of the case. Rushing cases may not be possible, so schedule the patient accordingly: (Laboratory time requirements are posted within the AEGD clinic).
- Please note that fixed cases that returned to the resident for final die trimming and identification of margins using a red pencil.
In-House Adjustments
- University of Maryland is fortunate to have in-house lab technicians who can do minor adjustment procedures; i.e., glazing a crown.
Remake Policies
- A re-make request form must be completed and signed by a full time faculty and the office manager before the case can be sent back to the lab. This is to verify the need for the re-make and to determine the onus of the financial responsibility.
- It is advised to remake impressions if remaking crown/bridge cases so as to avoid repeating the same error.
- All items from the first case must be returned to the lab, including the models and rejected restorations.
Restorative Materials and Equipment Used in the AEGD Clinic
Amalgam
Sybraloy
FastSet
Composite
TPH 3
Esthet X-Flowable
Esthet HD
Esthet XHD
Surefil SDR Flow
Glass Ionomers
- Fuji 9
Class V
Ketac
- Build Ups
FluoroCore II
KetacFil
- Liner
Vitrebond
Bonding Agents
Prime + Bond NT
Clearfil Repair
Photo Bond
Elect
Sealants
DeltonLC
Bleaching Solutions
- In Office
*Zoom
- Home Treatment
Night White Excel 16%
Temporary Crown Material
- Acrylic/Jet Alike
- Resin
Integrity
- Inlays
Fermit
Cementing Systems
- Without Bonding
Zinc Phosphate
Duralon
Fuji Cem
- With Bonding
Panavia F
Calibra
Variolink
Porcelain or Composite Veneers, Inlays and Onlays
Variolink
Calibra
Calibra Universal
Desensitizing Agents
Gel Kam
Protect
Duraphat
SE Bond
Post and Core Material
FluoroCore II
Amalgam
TPH Composite
ParaPost
Flexi-Post
Impression Posts/Cast Post
PINS: TMS (Regular and Minum)
Stabilok
Hemostatic Solutions
Hemodent
Visco Stat Plus
Impression Material
Alginate
Aquasil
Bite Registrations
Duralay
Regisil
Reline Materials
GC Reline (soft)
Coe-Soft (soft)
Coe-Comfort (soft)
UfiGel (hard C)
Temporary Cements
Duralon
Temp Grip
Endo Supplies
Ept, EndoIce
Apexlocator (RootZX)
Brassler Sequence
CaOH2
Cavit
Implants
3i Implant
ITI (Straumann)
Nobel Biocare
Miscellaneous
Perio: freeze dried bone
Graft material, endogain,
Cerec
Laser – Soft Tissue
Interra Chairside Occlusal Guard
Air Abrasion
- An air abrasion unit is available and it can be moved into the clinic as required. Unless familiar with the apparatus, a resident’s first use should be under close supervision of an attending who is comfortable with the equipment.
- Some of the many applications for air abrasion are:
- Removal of stains
- Preparation of pit and fissures prior to sealants
- Preparation of cavity preps that are small, including cervical abrasion sites
- Micro-etching porcelain for composite repairs
- But, NOT for amalgam removal
Clinical Intra-Oral Camera
There is one conventional clinical camera and an intraoral video camera available for documenting cases.
Residents must purchase a digital media compact flash (256 mb) for their own use.
Itero and Cerec 3D Systems
The AEGD clinic has an Itero system and Cerec 3D system. Training will be provided before the resident can use the system.
Documentation and Charts
Patient Chart Entries: All Patient Record entries require the use of the Assessment/Treatment/Evaluation Next Appointment (ATEN) system.
Standardized Format for Progress Notes
A standardized format for Progress Notes will be used for all patient record entries, except for Oral Surgery that already uses a standardized SOAP note. The “data elements” and “examples” of the Progress Note format are shown below.
Data Elements of Progress Note
| A: |
Assessment – reason for visit; pt. health/medical management considerations; consent |
| T: |
Treatment – concise and detailed description of procedures performed and medications |
| E: |
Evaluation – appraisal of treatment; patient’s reaction to treatment; extenuating circumstances |
| N: |
Next Visit – specific plans for next visit |
Examples of Progress Note
Date
| A: |
Patient presents for tx of occlusal caries on #19; no Changes in med. hx. since 1/15/99; pt. understands risks of today’s tx and reaffirms consent. |
| T: |
Mandibular block with 1.8 cc 2% Xylocaine; 1:100,000 epi.; rubber dam; #19 occlusal caries removal, CaOH2 (Dycal), Vitrebond, amalgam (Contour) restoration. |
| E: |
Patient apprehensive as usual regarding local anesthesia; deep caries approaching pulp, but no exposure; patient advised that tooth could need endodontic therapy; treatment completed. |
| N: |
6 month recall, check for caries progression on mesial of #3 by radiograph. |
Student Signature & #
Faculty Signature & #
Date
| A: |
Patient presents for SC/RP of ULQ; reports new RX, nifedepine for hypertension; BP right arm sitting: 145/80; pt. understands risks of today’s tx and reaffirms consent; plaque score: 65%. |
| T: |
Reinforced home care instructions, showed patient literature on gingival hyperplasia associated with nifedepine; local infiltration in area of #14 with 0.5ml of 2% Xylocaine with 1:100,000 epi.; ultrasonic removal of gross calculus followed by hand curette scaling and root planing; irrigated DL pocket of #14 with sterile saline. |
| E: |
Patient understands risk for hyperplasia, showed extra motivation to follow home care; 7mm pocket DL #14 difficult to complete instrumentation due to furcation; revaluation required. |
| N: |
Next visit 10/27/99: URQ SC/RP, whole mouth polish and fluoride; check tissue response and finish RP of distal furcation #14 before starting URQ. |
Student Signature & #
Faculty Signature & #
- At the end of each appointment period, all clinical services rendered during the appointment must be recorded on the "Continuation Sheet" of the patient's chart. This form must have a signature (no initials) and Provider Number recorded by the instructor supervising the student during the appointment period. An entry in Axium must be made for each appointment.
- Using the ATEN system of chart entries, the following information should be listed in the continuation notes: 1) date, 2) department, 3) tooth number, 4) diagnosis, 5) treatment listing all restorative materials (with brand names following each in parenthesis), 6) use of rubber dam, 7) appropriate remarks and/or post-operative instructions listed under E (Evaluation). Standard accepted abbreviations maybe used. Students and faculty must sign every entry and included their provider number.
Signatures
- All Daily Treatment Records MUST have an attending signature before the end of the day. Treatment Plans should have three signatures: patient, resident, and attending before treatment can begin.
- Prescriptions for narcotic-based medications must be signed by a Maryland licensed dentist who has a DEA number.
- Prescriptions for the laboratory work must be signed by the resident, the financial officer, and the faculty.
Guidelines for Completing a Medical Consultation Form
A. Reasons For Requesting a Medical Consultation
- Clarification of a specific condition or a specific drug therapy
- Clarification of a condition that may require pre-operative antibiotic coverage
- Requesting specific
- Laboratory test results, or
- Complete findings from a recent complete physical examination
B. Providing Information to the Consulting Healthcare Practitioner
- Oral diagnoses
- Use language suitable to the knowledge of the other healthcare provider
- Include all oral diagnoses
- Include some indication of the severity of each diagnosis
- i.e. “moderate to severe” periodontitis
- “1.5 cm.” squamous cell carcinoma with “associated lymphadenopathy”
C. Advising HCWs About Recommended Dental Treatment
- Include all foreseeable forms of treatment that may be employed
- All procedures that will cause significant bacteremia (e.g. deep scaling, C&B cord, etc.)
- All procedures that involve mucogingival surgery
- Biopsies, exodontia, implant placement
- All modes of anesthesia
- Local anesthetic; regional block anesthesia
- N2O, IVSD, general anesthesia
- Drug therapies: antibiotic pre-meds, antibiotic management of perio dx, alteration of Coumadin, Amicar
- This is the most important part of any medical consultation request
- It establishes, for the physician or other HCW, that you have been careful in:
- Taking a thorough patient history
Assessing the patient’s simple or complex medical status, AND MOST IMPORTANTLY
- That you have appropriately analyzed the significant medical factors in the patient’s history and FORMULATED A SPECFIC SET OF RELEVANT QUESTIONS.
- All medical consultations should be narrowly tailored to ask specific medical management questions that call for specific objective answers.
- Only if the objective data is particularly open to a fairly wide range of clinical judgment, should an opinion on that objective data be expressly requested by the dentist and given by the consulting physician or other HCW.
- Better medical consultations identify the dental management problem for the physician to consider, in the first line of this section, and then suggest a specific management approach to be used to ameliorate the problem.
- Example: 72 y.o. AA female è h/o MI x 3, CABG, and A-fib, on Coumadin.
- Must have patient’s INR 2.0-2.5 to proceed. If pt.’s INR is higher, we would normally D/C Coumadin 2 days prior to tx, do stat PT/INR the AM of tx, and resume Coumadin at the next scheduled dose. OK?
Please report the pt.’s most recent INR and advise.
- It is extremely important that a medical consultation reflects the patient’s comprehensive needs so that repeated consults are not required because the dental practitioner failed to think through potential medical complications which may arise with different modalities of treatment.
- Telephone consults are strongly discouraged!
- They should be limited to clarification of the physician’s recommendation, if it is illegible or contrary to regular regimens employed throughout Dentistry or Medicine.
- For example, chronic renal failure patients on hemodialysis may require a different antibiotic for SBE prophylaxis, and/or a different dosing regimen than other patients.
- A contemporaneous note in the chart should summarize this clarification of the initial consult.
D. The following patients may be unable to reliably relate their medical histories:
- Elderly
- Those suffering dementia or Parkinson’s disease
- Developmentally Challenged; Special Needs Patients
- Mentally Disable (psychosis patients)
- In these cases, the only reliable method for determining relative safety to treat is the Complete Physical Examination findings.
- The Complete Physical Examination
- Interpreting the Findings for Relative Safety to Treat the Dental Patient
- Who Cannot Reliably Relate a Medical History.
Outline of Physical Examination (HandPE)
- Vital signs: Temperature, pulse, blood pressure (both arms), respiratory rate. These observations need not be repeated under their respective subheadings.
- General appearance: state of orientation; development, state of nutrition, degree of discomfort, cooperativeness, other conspicuous general characteristics of appearance (including dress, neatness, behavior, gait and posture).
- Skin: color, temperature, texture, moisture, eruptions, ecchymoses or petechiae, hair distribution, nails. Significant scars.
- Head and face: Conformation, symmetry, abnormal movements, signs of injury, tenderness.
- Eyes: extraocular movements, sclerae, conjunctivae, pupils, (size, equality, regularity, reaction to light and accommodation), gross vision and visual fields.
- Ears: pinna, external canal, tympanic membrane, gross hearing, mastoids.
- Nose: obstruction, discharge, septal perforation or deviation. Sinus tenderness.
- Mouth: breath, mucous membranes, teeth, tongue, tonsils, faucial pillars, postnasal drip.
- Neck; stiffness, masses, venous distention, abnormal pulsations, thyroid, position of trachea; carotid bruits.
- Lymph nodes: size, consistency, tenderness, and mobility of cervical, supraclavicular, axillary, inguinal. (All nodes may be described here, or the regional nodes may be described with appropriate areas as examined.)
- Thorax: configuration, AP diameter, symmetry, and amplitude of motion.
Breasts: masses, tenderness, discharge from nipples, areolae.
- Lungs:
Inspection: respiratory excursion, rhythm, symmetry.
Palpation: fremitus (tactile).
Percussion: resonance, lung borders and descent.
Auscultation: breath sounds, spoken and whispered voice sounds (vocal fremitus), rales, friction rubs.
- Heart:
Inspection: Precordial movements, precordial bulging.
Palpation: apex impulse and PMI, thrills, shocks.
Percussion: Heart borders, sternum.
Auscultation: rhythm, heart sounds, murmurs (include left lateral position and sitting in full expiration), friction rubs, extracardiac.
- Abdomen:
Inspection: contour, engorged veins, protrusions, umbilicus, visible peristalsis.
Percussion: Hepatic, splenic, bladder dullness, gaseous distention, shifting dullness.
Auscultation: peristaltic sounds, vascular bruits.
Palpation: tenderness, rebound tenderness, rigidity, fluid wave, liver, spleen, kidney masses, hernias. If liver or spleen are palpable, note character or edge. Costovertebral tenderness.
- Spine: Vertebral curvatures, mobility, tenderness.
- Extremities:
Joints: swelling, effusion, deformities, tenderness, increased warmth, mobility. Clubbing, cyanosis, edema. Calf tenderness, Homan's sign. Character and equality of radial, femoral, posterior tibial and dorsalis pedis pulses; sclerosis of arterial walls; abnormal venous structures (varicosities, telangiectases).
- Neurological: A limited or screening neurological examination is part of every routine physical examination. When positive findings make a more complete study necessary, the complete examination is done. Mental status; gait and station, abnormal movement; cerebellar signs; cranial nerves; muscle strength, atrophy, fasciculations; sensation: touch, pain, vibration, position sense; reflexes: (biceps, triceps, Hoffman, abdominals, cremasterics, knee jerks, ankle jerks, plantar); meningeal irritation (nuchal rigidity, Kernig's sign).
- Genitalia:
- Male: penis, scrotum, testes, epididymis, spermatic cord. Discharge, inguinal canals.
- Female: speculum examination of vagina and cervix, palpation of uterus and adnexa. Pap smears, culture when indicated.
- Rectal: External hemorrhoids, fissures.
Digital: Sphincter, hemorrhoids, prostate, seminal vesicles (or uterus and cervix), Feces (description of gross appearance) and test for occult blood.
* Summary
Concise summary of relevant points in history and physical examination.
* Formulation
This is intended to alert the reader to the basis on which the diagnoses were made and the direction in which the work-up will process.
It is a statement of what the leading diagnoses are, which diagnoses you favor and why, how you will differentiate between the likely diagnoses and a general approach to therapy, if there is a presumptive diagnosis.
Diagnosis: _______________________________________________________
Plans for further investigation and management: __________________________________________________________________________________________________________________
Introduction to Treatment Planning Technical Criteria
Format for Comprehensive Treatment Plan Work Up
I. History (S)
- Chief Complaint (CC)
- It should be a symptom - record the patient’s impression of disease/problem in his/her own words.
- History of Present Illness (HPI)
- Record details of chief complaint and related complaints - history of chief complaint.
- Past Medical History (PMH)
- Record health history of systemic conditions, injuries, and hospitalizations in detail - medical consultation is present, if indicated.
- Childhood diseases
- Serious illnesses/transfusions
- Family health history which may bear on patient’s present or future health status
- Allergies and sensitivities
- Current medications
- Review of systems (ROS)
- Environmental/social history
- Describe in detail any environmental factors that could impact on diagnosis and treatment planning, i.e., alcohol intake, tobacco usage, vocation, finances, etc.
- Dental History
- Describe in detail the patient’s awareness of and involvement in previous dental treatment.
- Family dental health history (parents, siblings, spouse, children)
- Oral hygiene habits
II. Examination - Findings; list problems requiring attention, all of these must be addressed in TX sequence; charting must be complete - (O)
- List general observations and systemic findings - age, vital signs, skin, limbs, development nutrition.
- Record oral and extraoral findings: perform a thorough examination of the head, neck, face, and oral tissues.
- Head, neck, eyes, ears, nose, skin and secretions
- Lips, oral mucus, palate, pharynx, tongue and floor of mouth
- Gingival - color, texture, consistency, contour, amount of keratinized tissue, bleeding; details of periodontal condition on appropriate form
- Occlusion/musculature - a general statement of condition; details on appropriate form
- Dentition - a general statement of condition; details on appropriate form
- Oral hygiene - a general statement of condition; details on appropriate form
- Radiographic Findings
- Obtain indicated radiographs which my include the following:
- periapical films (full mouth survey)
- posterior bitewing films
- panoramic film
- any necessary supplemental films
- Microscopic - if indicated, obtain a phase contrast evaluation of microflora
NOTE: The case is mounted on an articulator, all required radiographs, laboratory and clinical tests are obtained.
III. Diagnosis - (A)
- List disease processes and abnormalities that address all pertinent findings.
- Systemic diagnosis
- Dental diagnosis
IV. Treatment Objectives - (A)
- Make a general statement of the desired goals of treatment taking into account the findings, the patient’s situation and the resources of the practitioner. List considerations:
- Patient health
- Patient desires
- Patient age
- Patient financial restraints
- Prognosis (long and short term)
- Provider skills
- Devise ideal (long-term) treatment objectives and immediate objectives (if applicable) that will support the ideal; formulate a segmented (progressive) treatment plan. Discuss all treatment options with the patient.
- All fees for all treatment must be listed when the treatment plan is presented to the patient.
V. Planned Treatment Sequence - (P)
(The Written Treatment Plan)
- A planned, well organized sequence of treatment is listed according to treatment phases that addresses all diagnosis and pertinent findings; materials to be used and alternate treatment plans are listed; best treatment plan for that individual patient is presented.
- Order of treatment (Enter Each Phase - e.g., If N/A Enter “Phase 1 - N/A”)
- Systemic phase
Systemic health considerations. Consult with physician when in doubt. Determine need for premedication, diet, precautions to protect patient and dental team, etc.
- Acute Urgent phase
Treat problems of acute pain, bleeding, lost restorations, etc.
- Disease Control Hygienic phase (most import phase - steps necessary to control disease) for this specific patient generally in the order listed:
- Patient education and instruction in plaque control; fluoride program
- Biopsies if necessary
- Preliminary gross scaling - if necessary
- Caries control, and endodontic therapy
- Extraction of hopeless teeth. Temporary CPD’s and RPD’s if needed.
- Root planning
- Maintain plaque control
- Preliminary occlusal adjustment if indicated
- Minor tooth movement/orthodontic treatment
- Occlusal splints if indicated
- Definitive occlusal adjustment when necessary
- Continuous evaluation of oral hygiene and tissue response, and reassessment of the entire treatment plan
- Definitive/Corrective phase: correct environment to allow patient to maintain good oral hygiene
- Hemisections with temporary splinting
- Periodontal surgery, bone and soft tissue grafting
- Treatment of hypersensitive teeth
- Implants
- Restorative dentistry (should wait at least two months following extensive surgery)
- Recheck and refine occlusion
- Maintenance phase:
- Re-examine for effectiveness of plaque control, recurrence of periodontal disease, caries, and occlusal problems: reinforce oral hygiene instruction, perform prophylaxis including topical fluoride application. Recall based on the specific patient’s needs.
- Complete periodic radiographic survey of the dentition if indicated. Compare with prior radiographs
- Recheck prosthetic treatment
- Treatment of any active periodontal disease
- Treatment of recurrent carious lesions
- Endodontic therapy if pulpal and/or periapical lesions have developed or not resolved
- Replacement of restorations which no longer satisfy health, function or esthetic requirements
- Make new occlusal splints when old ones are broken down, worn out or lost
VI. Prognosis
- State a prediction, based on an educated calculation, of the response of hard and soft tissue to the treatment planned, both long and short term.
VII. Signing the Treatment Plan
- The patient must sign the treatment plan prior to any treatment being rendered. This is to establish that the patient accepts the treatment plan. The resident and faculty member should also sign the treatment plan.
Periodontal Screening & Recording System (PSR)
Example of Monthly Production Report
| Provider |
Revenue Budget March |
Actual Revenue March |
Budget Variance |
Revenue Budget |
Actual Charges March |
Budget Variance |
YTD Budget |
YTD Actual Revenue |
YTD Budget Variance |
| Resident |
|
|
|
|
|
|
|
|
|
|
$3,800 |
$2,665 |
($1,145) |
$3,800 |
$2,983 |
($817) |
$29,100 |
$19,415 |
($9,685) |
|
$3,800 |
$3,562 |
($238) |
$3,800 |
$3,984 |
$814 |
$29,100 |
$32,389 |
$3,289 |
|
$3,800 |
$3,721 |
($79) |
$3,800 |
$1,724 |
($2,076) |
$29,100 |
$24,059 |
($5,041) |
|
$3,800 |
$3,001 |
($799) |
$3,800 |
$4,323 |
$523 |
$29,100 |
$20,914 |
($1,846) |
|
$3,800 |
$5,006 |
($1,206) |
$3,800 |
$6,783 |
$2,983 |
$29,100 |
$31,535 |
$2,435 |
|
$3,800 |
$3,954 |
$154 |
$3,800 |
$4,570 |
$770 |
$29,100 |
$27,254 |
($1,846) |
|
$3,800 |
$2,051 |
($1,749) |
$3,800 |
$2,118 |
($1,682) |
$29,100 |
$14,694 |
($14,406) |
|
$3,800 |
$4,431 |
$631 |
$3,800 |
$5,155 |
$1,355 |
$29,100 |
$32,348 |
($3,248) |
|
$3,800 |
$5,119 |
$1,319 |
$3,800 |
$7,278 |
$3,478 |
$29,100 |
$27,100 |
($2,100) |
|
$3,800 |
$3,984 |
$184 |
$3,800 |
$5,656 |
$1,856 |
$29,100 |
$19,414 |
($9,686) |
|
$3,600 |
$4,105 |
$505 |
$3,600 |
$3,613 |
$13 |
$27,000 |
$23,517 |
($3,483) |
|
$3,600 |
$1,398 |
($2,202) |
$3,600 |
$893 |
($2,707) |
$27,000 |
$18,047 |
($8,953) |
|
$3,400 |
$2,181 |
($1,219) |
$3,400 |
$1,415 |
($1,985) |
$25,500 |
$15,573 |
($9,927) |
|
$3,400 |
$2,967 |
($433) |
$3,400 |
$3,341 |
($59) |
$25,500 |
$15,573 |
($9,927) |
|
$3,200 |
$2,620 |
($580) |
$3,200 |
$3,401 |
$201 |
$24,000 |
$14,580 |
($9,420) |
|
$3,200 |
$3,351 |
$151 |
$3,200 |
$1,889 |
($1,311) |
$24,000 |
$17,904 |
($6,096) |
|
$3,200 |
$3,174 |
($26) |
$3,200 |
$3,007 |
($193) |
$24,000 |
$21,092 |
($2,908) |
|
$3,200 |
$4,472 |
$1,272 |
$3,200 |
$4,925 |
$1,725 |
$24,000 |
$23,198 |
($802) |
|
$3,200 |
$1,426 |
($1,774) |
$3,200 |
$1,392 |
($1,808) |
$24,000 |
$10,164 |
($13,836) |
|
$3,200 |
$1,324 |
($1,876) |
$3,200 |
$1,421 |
($1,779) |
$24,000 |
$17,004 |
($6,996) |
Production Report
Treatment Details by Provider from 02-Nov-2003 to 30-Nov-2003
AGD-R- AGD Resident Activity
| Provider |
Procedure |
TX# |
RVU |
Amount |
| ROO327-Mel G |
D0120-Periodic oral evaluation |
2 |
0.00 |
60.00 |
|
D0140-Limited oral eval-prob focused |
3 |
0.00 |
135.00 |
|
D0150-Comprehensive oral eval |
16 |
0.00 |
720.00 |
| |
D0210-Intraoral-complete series |
9 |
0.00 |
720.00 |
| |
D0220-Intraoral-periapical 1st film |
3 |
0.00 |
51.00 |
| |
D0274-Bitewing-4 films |
3 |
0.00 |
117.00 |
| |
D0330-Panoramic film |
1 |
0.00 |
75.00 |
|
D1110-Prophy-adult |
3 |
0.00 |
171.00 |
|
D1351-Sealant-per tooth |
2 |
4.00 |
66.00 |
|
D2330-Resin-based comp-1 surf, ant |
8 |
48.00 |
520.00 |
|
D2331-Resin-based comp-2 surf, ant |
10 |
90.00 |
750.00 |
|
D2332-Resin-based comp-3 surf, ant |
2 |
22.00 |
200.00 |
|
D2335-Resin-based comp-4+ surf, ant |
3 |
42.00 |
363.00 |
|
D2391-Resin-based comp-1 surf, post. |
3 |
18.00 |
225.00 |
|
D2392-Resin-based comp-2 surf, post. |
1 |
9.00 |
95.00 |
|
D2393-Resin-based comp-3 surf, post. |
2 |
22.00 |
240.00 |
|
D2759.1-Start Procedure |
2 |
0.00 |
0.00 |
|
D2751.1-Start Procedure |
1 |
0.00 |
0.00 |
|
D2940-Sedative Filling |
1 |
2.00 |
45.00 |
|
D2950-Core buildup-including pins |
1 |
14.00 |
119.00 |
|
D2954-Prefab post and core |
1 |
5.00 |
140.00 |
|
D33191,1-Start Procedure |
1 |
0.00 |
0.00 |
|
D3320.1-Start Procedure |
2 |
0.00 |
0.00 |
|
D3320.2-Complete Procedure |
2 |
0.00 |
0.00 |
|
D3320-Endo therapy-bicuspid |
2 |
0.00 |
750.00 |
|
D4263-Bone repl graft – 1st site/quad |
1 |
0.00 |
90.00 |
|
D4-266-Guided tissue regen-resorb |
1 |
0.00 |
385.00 |
|
D5110.1-Start Procedure |
1 |
0.00 |
0.00 |
|
D5214.1-Start Procedure |
1 |
0.00 |
0.00 |
|
D5630-Repair or replace broken clasp |
1 |
2.00 |
105.00 |
|
D5640-Replace teeth-per tooth |
1 |
0.00 |
70.00 |
|
D6240.1-Start Procedure |
2 |
0.00 |
0.00 |
|
D6750.1-Start Procedure |
2 |
0.00 |
0.00 |
|
D7140-Extraction, eruptd tth/exp rt |
11 |
0.00 |
803.00 |
|
D9430-Office visit-observation only |
1 |
0.00 |
28.00 |
|
D9972-External bleaching-per arch |
2 |
4.00 |
290.00 |
| R00327-Mel G Totals |
108 |
282.00 |
7,333.00 |
Treatment Requirements
Treatment Requirements