Directions for Patient Data Forms
Periodontal Assessments:
Periodontal assessments are performed to identify patients’ periodontal health status.
Review previous periodontal assessments, compare with current data to identify changes.
Please view the link below to review how to perform an EIOE exam, pulp testing and the numerous elements of the clinical data forms, including the periodontal assessment form in the UMB Dental charts.
http://dentalweb.umaryland.edu/tpw/introduction.html
When the periodontal form is completed for a new patient:
- Document “everything”. A comprehensive periodontal charting must be done every three years for recall patients.
When the periodontal form is completed for a recall patient:
- Document existing restorations and any new hard tissue findings (caries, broken restorations, new restoration etc.) at every recall visit on a new form
- EPR: update the existing HTC. EPR provides you with the opportunity to view HTC saved at different periods of time.
- Probe all the teeth, but record only probe readings (PD) that are ≥ 4mm at every recall visit on a new form
- Record all readings (CEJ-GM, PD, AL) on teeth with probe depths (PD) ≥4mm for all recall patients.
- Record all readings on teeth with areas of recession (+ CEJ-GM readings) that have CHANGED since the previous charting.
- Record all bleeding sites.
Periodontal Classification:
To determine CAL, document the CEJ- GM reading, the probing depth (PD), and ADD or SUBTRACT to calculate the attachment level (CAL)*
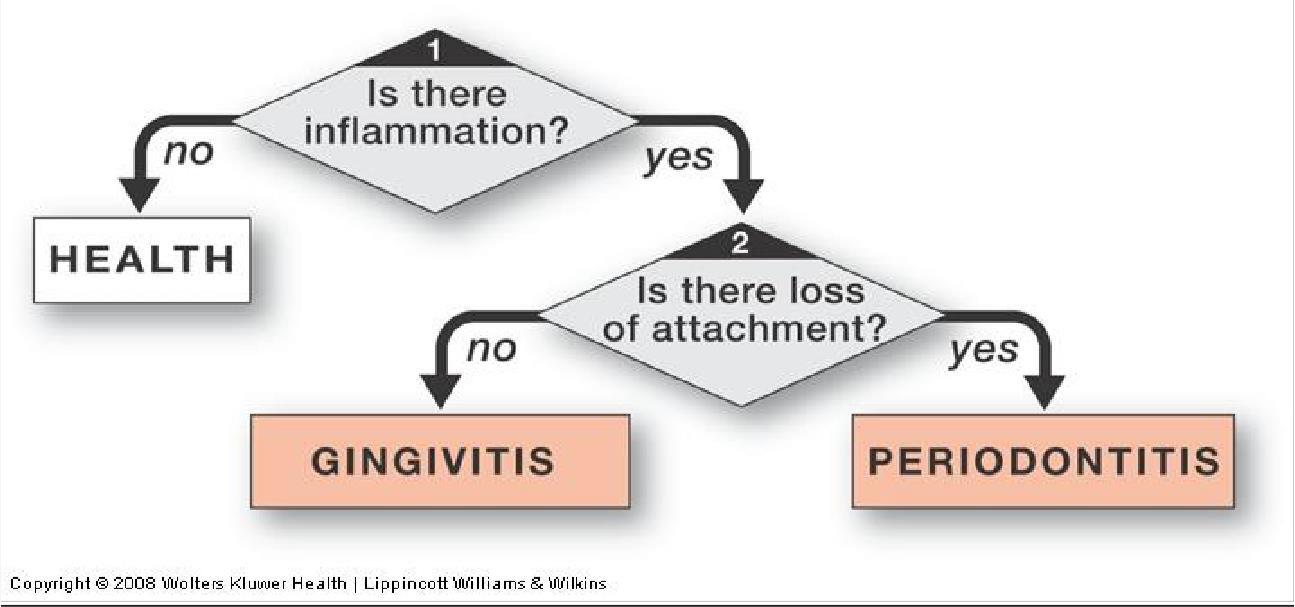
Health –No inflammation or ≥4 mm probe depths
Periodontal Disease:
Gingivitis – Inflammation- erythema and/or edema, no 4 mm probing depths, bleeding on gentle probing, no attachment loss
Periodontitis- a combination of
- Inflammation
≥4 mm probe depths
- Attachment loss
Only those areas with probing depths of 4mm or more are classified as periodontal disease. Once periodontal disease been determined classify in terms of:
- Extent*
* Localized less than 30% of teeth present
* Generalized ≥ 30% of teeth present
*Classify EXTENT for Gingivitis also
- Severity Clinical Attachment Loss/Level (CAL)
| * Mild |
=1-2mm |
| * Moderate |
= 3-4mm |
| * Severe |
≥ 5mm or more |
Types of Periodontitis:
- Chronic Periodontitis (most periodontitis patients are classified in this category)
- Aggressive Periodontitis
- Periodontitis as a Manifestation of Systemic Disease
- Necrotizing Periodontal Diseases
- Abscesses of the Periodontium
- Periodontitis as a result of Endodontic lesions
- Developmental or Acquired Deformities and Conditions
- Refractory Periodontitis
How to Chart
- Chart all missing teeth
- Record both the Probing Depth (PD) and the distance from the gingival margin (GM) to Cemento-enamel Junction (CEJ).
For teeth with crowns, use the crown margin as the CEJ. For other situations, estimate where the CEJ is (e.g., cervical composites) or mark with an “X” if it is no longer discernable (e.g., fractured tooth).
If the CEJ is apical to GM (inflammation), include a minus sign (-) next to the number. If the CEJ is coronal to the GM (recession), do NOT include a minus sign.
- To record the clinical attachment level (CAL), add the CEJ-GM reading to the PD:
- CEJ–GM reading of (-1mm) + PD of 4mm = CAL of 3 mm (-1 + 4 = 3mm)
- CEJ-GM reading of 2mm + PD of 4mm = CAL of 6mm (2 + 4 = 6mm).
- Record the keratinized gingival (KG) reading. Measure it in mm from the GM to the mucogingival junction (MGJ). Record one score for the facial surface on the maxillary and mandibular arches.
- Complete a gingival description and calculate bleeding index. Bleeding Index = # of bleeding points divided by # of possible sites x 100%.
Gingival Description Guideline
| Description |
Within Normal Limits |
Deviation From Normal |
| Color |
Melanin Pigmentation
Coral pink |
Pallor
Erythema
Cyanosis |
| Consistency |
Firm/Resilient
Attached gingiva, firmly bound
Alveolar Mucosa- mobile |
Edematous-soft, spongy
Hyperplastic Flaccid/retractable
Fibrotic- firm, hard |
| Surface Texture |
Attached gingiva- stippled |
Loss of stippling
Heavy stippling |
| Contour |
Marginal gingiva-knife edged, follows curve of tooth
Papillae- pyramidal, fills interproximal space, open contacts- flat/saddle shape |
Marginal Gingiva- rounded, rolled, clefts
Papillae- blunted, bulbous, cratered, flattened |
| Width of Attached Gingiva |
Width of attached gingiva > or = 1 mm |
Width of attached gingiva < 1 mm |
Patient Difficulty Determination
Department of Dental Hygiene
Baltimore College of Dental Surgery
University of Maryland at Baltimore
Guidelines for Determining Case Difficulty Level
| Accretion Levels Stain |
| |
L |
M |
H |
| light colored linear and/or diffuse |
X |
|
|
| dark colored linear and/or diffuse |
X |
X |
|
| brown/black leathery |
|
X |
|
| Supramarginal Calculus |
|
L |
M |
H |
| light, scattered spicules |
X |
|
|
| fine, continuous band of calculus at gingival 1/3 |
X |
|
|
| veneer of calculus covering up to 2/3 of the clinical crown |
x |
x |
x |
| continuous band of dense calculus covering up to 2/3 clinical crown |
|
X |
X |
| bulky, ledge-like mass deposit covering up to 2/3 of clinical crown |
|
|
X |
| gross, bulky mass (“calculoma”) may or may not extend to occlusal surface |
|
|
X |
| Submarginal Calculus |
|
L |
M |
H |
| discrete, scattered spicules |
X |
X |
|
| isolated projection/individual nodules |
|
X |
|
| continuous band of dense calculus |
|
X |
X |
| isolated areas of burnished/veneer calculus |
|
X |
X |
| bulky, ledge-like mass |
|
|
X |
Instrumentation associated with Case Difficulty Levels*
| L- |
Light scaling required, or may include minimal root planing |
| M- |
Moderate scaling required including |
| H- |
Moderately extensive/extensive scaling required and/or generalized |
*Difficulty level is determined by assessing both the quantity and quality
Hard Tissue Charting Codes
Click TX History tab --->
Chart add icon (on right) -->FINDINGS (on left)
Chart note entries in the EPR
While there are templates for chart notes in the EPR, chart notes should be written in the standard dental school form including all areas of the S.O.A.P. format as follows:
S=Subjective
What the patient tells you
Patient’s chief complaint, history of present illness (this complaint) Past medical history, past dental history
Example: Patient presents complaining of missing tooth #7. States that the tooth was extracted after an unsuccessful attempt at restoration (use quotations when appropriate). Past medical history is non-contributory, however patient admits to smoking 1/2 pack per day of cigarettes. Past dental history: Patient receives dental cleanings irregularly, does not use floss.
O=Objective
- what you see in your examination, including radiographic
- information obtained in your EIOE, gingival/perio assessment, HTC, etc.
- radiographic findings bone levels, caries, pathology
Example: Intra-oral exam reveals tongue, palate, FOM WNL. Gingiva is pink and stippled with localized swelling and redness in lower anterior and maxilla posterior regions. Pocketing and dentition as charted (see charting). Missing tooth #7. Adjacent teeth #6, 8 show slight drifting into space of #7. Slight plaque, moderate stain.
Slight stick to explorer in occlusal pits maxillary premolars, however bite-wing radiographs reveal no sign of decay. #31 with large IRM. Radiographic exam reveals IRM #31 is close to pulp. Bone loss seen in area of #23- 26.e
A=Assessment
- problem list, or diagnoses. It works well to number these and make corresponding remarks in the '"'Plan'"' section.
Example:
- Missing #7
- Localized periodontal disease #23-26
- #31 restoration close to pulp, poss. pulpal pathology
- Max. premolars non-carious
P=Plan
- what you plan to do, and what you did today. Try to address each problem.
- Patient disposition pleasant, agitated, friendly, etc.
- Interval of recall 3 mo recall
- Planned treatment for next visits Ex, perio main, 4BW
- Referrals to other departments OS for evaluation of lesion R lateral border of the tongue
- Areas that require re-evaluation check 2 M incipiency on next BW
- All services rendered
Include instrumentation, methods and materials used. Such as 4 vertical BW exposed, scaled/Root planned maxillary molars with Gr11/12, 13/14, scaled all other teeth with Un 13/14,204S, rubber cup polish with extra fine paste, dried all teeth and placed 5% Fluoride Varnish. Gave post treatment instructions.
- Local and/or topical anesthesia used
Type, method of delivery, amount and with or without epinephrine (amount of epi). Obtain signature of student (if other than yourself) or faculty who administered the anesthetic.
- Any recommendations made by student or faculty
Homecare, dietary counseling, habit modifications, referrals, etc.
Include anticipated outcome of your recommendations and the mechanism of measurement.
- Note that radiographs were evaluated by dental faculty when applicable
Example:
Today: Examination, full mouth series radiographs taken and read. Alg. imps for study
- Explained to patient that there are several different ways to restore missing #7. Will review study casts and discuss options and fees at next appointment.
- Expl'd to patient need for more frequent prophy, and the use of floss.
- Will eval pulpal status of #31 with endodontic consult
- Recommend no treatment for occlusal fissures of premolars RTC (Return to clinic) Discuss treatment plan options. Chart entries for initial visits, periodic evaluations, and emergency visits are well understood and legally complete if written in the form of a SOAP note. Subsequent treatment visits do not need such detail.
ALWAYS HAVE ALL FACULTY AND STUDENTS THAT WORKED WITH THE PATIENT SWIPE IN AXIUM.
ALWAYS DOCUMENT IF PATIENT ARRIVED LATE, CANCELLED OR DID NOT SHOW FOR AN APPOINTMENT AND ANY PHONE CALLS YOU MADE TO THEM REGARDING THE APPOINTMENT.