Periodontal Assessments:
Periodontal assessments are performed to identify patients’ periodontal health status.
Review previous periodontal assessments, compare with current data to identify changes.
Please view the link below to review how to perform an EIOE exam, pulp testing and the numerous elements of the clinical data forms, including the periodontal assessment form in the UMB Dental charts.
http://dentalweb.umaryland.edu/tpw/introduction.html
When the periodontal form is completed for a new patient:
- Document “everything”. A comprehensive periodontal charting must be done every three years for recall patients.
When the periodontal form is completed for a recall patient:
- Document existing restorations and any new hard tissue findings (caries, broken restorations, new restoration etc.) at every recall visit on a new form
- EPR: update the existing HTC. EPR provides you with the opportunity to view HTC saved at different periods of time.
- Probe all the teeth, but record only probe readings (PD) that are ≥ 4mm at every recall visit on a new form
- Record all readings (CEJ-GM, PD, AL) on teeth with probe depths (PD) ≥4mm for all recall patients.
- Record all readings on teeth with areas of recession (+ CEJ-GM readings) that have CHANGED since the previous charting.
- Record all bleeding sites.
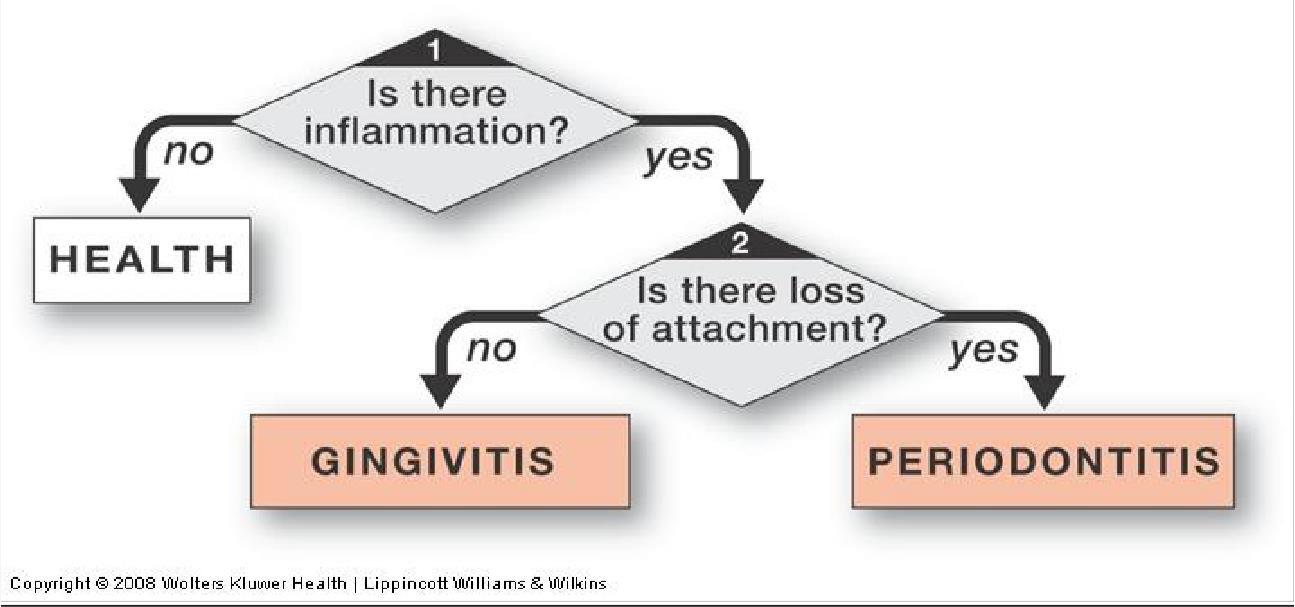
Periodontal Classification:
To determine CAL, document the CEJ- GM reading, the probing depth (PD), and ADD or SUBTRACT to calculate the attachment level (CAL)*
Health –No inflammation or ≥4 mm probe depths
Periodontal Disease:
Gingivitis – Inflammation- erythema and/or edema, no 4 mm probing depths, bleeding on gentle probing, no attachment loss
Periodontitis- a combination of
- Inflammation
≥4 mm probe depths
- Attachment loss
Only those areas with probing depths of 4mm or more are classified as periodontal disease. Once periodontal disease been determined classify in terms of:
- Extent*
* Localized less than 30% of teeth present
* Generalized ≥ 30% of teeth present
*Classify EXTENT for Gingivitis also
- Severity Clinical Attachment Loss/Level (CAL)
| * Mild |
=1-2mm |
| * Moderate |
= 3-4mm |
| * Severe |
≥ 5mm or more |
Types of Periodontitis:
- Chronic Periodontitis (most periodontitis patients are classified in this category)
- Aggressive Periodontitis
- Periodontitis as a Manifestation of Systemic Disease
- Necrotizing Periodontal Diseases
- Abscesses of the Periodontium
- Periodontitis as a result of Endodontic lesions
- Developmental or Acquired Deformities and Conditions
- Refractory Periodontitis
How to Chart
- Chart all missing teeth
- Record both the Probing Depth (PD) and the distance from the gingival margin (GM) to Cemento-enamel Junction (CEJ).
For teeth with crowns, use the crown margin as the CEJ. For other situations, estimate where the CEJ is (e.g., cervical composites) or mark with an “X” if it is no longer discernable (e.g., fractured tooth).
If the CEJ is apical to GM (inflammation), include a minus sign (-) next to the number. If the CEJ is coronal to the GM (recession), do NOT include a minus sign.
- To record the clinical attachment level (CAL), add the CEJ-GM reading to the PD:
- CEJ–GM reading of (-1mm) + PD of 4mm = CAL of 3 mm (-1 + 4 = 3mm)
- CEJ-GM reading of 2mm + PD of 4mm = CAL of 6mm (2 + 4 = 6mm).
- Record the keratinized gingival (KG) reading. Measure it in mm from the GM to the mucogingival junction (MGJ). Record one score for the facial surface on the maxillary and mandibular arches.
- Complete a gingival description and calculate bleeding index. Bleeding Index = # of bleeding points divided by # of possible sites x 100%.